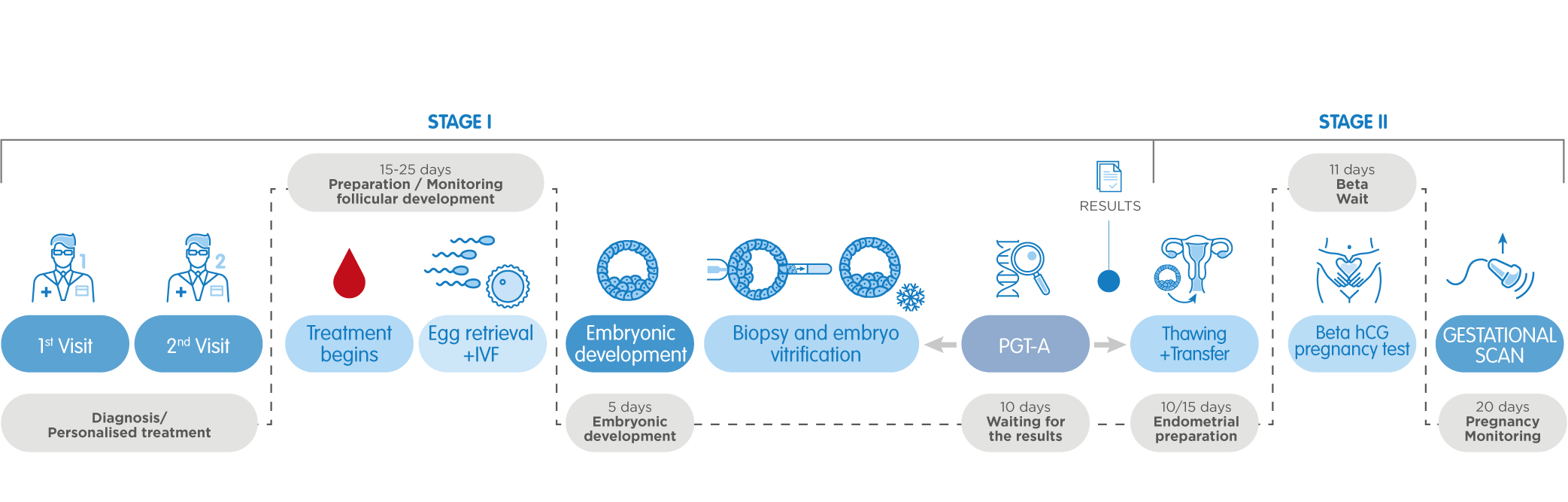
Preimplantation genetic testing, or PGT, comprises a group of genetic assays used to evaluate embryos produced through in vitro fertilization before transfer to the uterus.
The method allows to discard embryos with serious genetic disorders to ensure that children are born free of hereditary diseases.
The core of the method
PGT is applicable for a range of genetic problems that can cause implantation failure, miscarriage and birth defects in a resulting child. Such genetic defects may include a missing or an extra chromosome in the embryo, single gene disorders, or the rearrangement of genes. Depending on the type of problem to be detected, various variants of PGT are performed.
Types of abnormalities
Chromosomes are threadlike structures found in the nucleus of every cell and containing genetic information in the form of single, long DNA molecule. DNA, in turn, is organized in genes, basic physical unit of inheritance. They contain the information needed to specify traits. Humans have approximately 20,000 genes.
Chromosomes are categorized into autosomes (the first 22 pairs) and a pair of sex chromosomes (XX in the case of women and XY in men).
Each parent contributes one chromosome to each pair so that the child receives half of their chromosomes from their mother and half from their father.
However, sometimes a change may occur in a chromosome leading to a chromosomal abnormality.
Those abnormalities that imply an extra or a missing chromosome are referred to as numerical. Other abnormalities are structural, at which a part of an affected chromosome can miss, break off, be duplicated, inverted or transferred onto a different chromosome.
In other cases, changes occur in a DNA sequence and affect specific genes. Most mutations have no effect over the performance of the organism, but some of them impedes normal functioning.
If such genetic alteration takes place in the eggs or sperm, it can be passed on to the child.
Types of PGT and Indications
1. Preimplantation Genetic Testing for aneuploidy (PGT-A testing).
During this procedure, the embryo produced during IVF is analyzed to detect possible extra or missing chromosomes, the state also called aneuploidy. Aneuploidy is responsible for the vast majority of first trimester miscarriages and is most frequently incompatible with life. Those that do not lead to abortion are associated with genetic disorders like Down syndrome (duplication in the chromosome 21).
Other chromosomal aneuploidies which result in genetic disorders include trisomy 13 (Patau syndrome), trisomy 18 (Edwards syndrome), or 45X (Turner syndrome).
PGT-A is recommended for:
- Women at the age of 35 or higher;
- Women with recurrent implantation failure;
- Couples with normal karyotypes (the number and visual appearance of the chromosomes) who have experienced recurrent miscarriage;
- Couples with suspected or diagnosed male factor (substantial alterations of sperm parameters may indicate the presence of an aneuploidy in the sperm cells);
- Couples who experienced an altered number of chromosomes during a previous pregnancy;
- Couples where one or both partners are carriers of numerical abnormalities in the sex chromosomes.
- Preimplantation genetic testing has helped many couples to prevent the birth of children with severe genetic diseases. No one should be surprised that the frequency of use for this method is increasing.
2. Preimplantation Genetic Testing for monogenic disorders (PGT-M)
PGT-M is a genetic test performed on embryos produced through IVF. This method was developed to help people who know they risk to pass on a specific single gene disorder to their children:
- Couples in which one of the partners is diagnosed with a genetic disorder;
- Couples in which both partners are unaffected carriers of the same genetic condition;
- People with family history of a genetic disorder.
Indications
- Both partners in the couple are carriers of the same autosomal recessive disorders (e.g. Cystic fibrosis);
- One of the partners is a carrier of an X-linked disorders (e.g. Duchenne Muscular Dystrophy);
- One of the partners is diagnosed with an autosomal dominant disorders (e.g. Huntington disease);
- One of the partners has a mutation associated with a hereditary cancer syndrome (e.g. BRCA1 & 2);
- A previous pregnancy with a single gene disorder.
Passing on a single-gene disorder obeys the principles of Mendelian inheritance. It means, a certain trait is controlled by a single gene with two alleles, one of which may be dominant to the other, called recessive.
An autosomal dominant disorder may be inherited according to the following pattern – one of the partners carries one affected allele and suffers from the disease, and the other partner's gene is unaffected. In accordance with Mendelian inheritance, 50% of their children will be unaffected and 50% will inherit the responsible gene and develop the disorder.
Autosomal recessive disorders requires two recessive alleles to translate into a disease. Accordingly, both the maternal and the paternal DNA must have the responsible allele. In the case when both parents are carriers (have one dominant and one recessive allele), the inheritance will follow this scheme – 25% of the children will be completely unaffected (inherit two dominant alleles), 50% will become carriers, and 25% will suffer form the disorder (inherit two recessive alleles).
In both cases, PGT-M allows to select the embryos who have only healthy versions of the gene.
3. Preimplantation Genetic Testing for structural rearrangements (PGT-SR)
This genetic test is targeted at determining whether embryos produced through IVF have chromosomes that are arranged abnormally or are not sized correctly.
Chromosomal structural rearrangements may occur due to a rupture or incorrect union of various segments of a chromosome. They can be balanced (the amount of genetic information is correct, but some of this information is in disarray) or unbalanced (the amount of information is incorrect). People with such disorders are at risk of producing embryos with the incorrect amount of genetic material. Embryos with such abnormalities do not normally develop in successful pregnancies.
Indications
PGT-SR is a suitable option for people with a chromosome rearrangement.
Chromosomal structural rearrangements:
This group of mutations encompass a number of events.
Translocation is a balanced rearrangement at which a segment of a chromosome breaks off and attaches on another location. Reciprocal translocations (when two segments within one chromosome pair change places) are the most common structural chromosome abnormality – it is found in 0.2% of newborns.
Deletion is the loss of a segment of a chromosome. While a chromosome has specific mechanisms to reconstuct itself, two segments on either side of the deleted one get assembled. However, a significant part of genetic material is missing.
Duplication means that a segment of a chromosome repeats itself, resulting in extra genetic material in the region. The duplicated segment can be located adjacent to original (tandem duplication), or in a different region of the same chromosome or even on another chromosome (insertional duplication).
Insertion occurs when a segment detaches from its usual location on a chromosome and reattaches to another chromosome.
When a ring is formed, both ends of a chromosome break off and fuse together trying to repair itself. It implies that a substantial amount of genetic information (which was located at the ends of the arms of the chromosome) is missing. The genes remaining on the chromosome cannot function properly, which manifests itself as a disease.
Inversion is a chromosomal mutation that occurs when a part of a chromosome breaks off, rotates through 180 degrees and reattaches in the same location. Depending on the type, the resulting rearrangement may be either balanced, or unbalanced.
Structural chromosomal rearrangements that contain at least three breakpoints with exchange of genetic material between two or more chromosomes are referred to as complex chromosomal rearrangements and occur rarely.